Premature rupture of membrane (PROM) is a condition where a membrane rupture that occurs before the onset of labor. Its incidence is 8 – 10%.
Preterm PROM – if premature rupture of membrane occurs before 37 gestestional age. Its incidence is 1%.
Latency period – it is the time gap from the membrane rupture to delivery. Latency period increase with decreasing gestestional age. Eg:- at term, half of the cases will deliver within 5 hours and 95% will deliver within 28 hours. But if premature rupture of membrane occurs before 34 weeks, 93% of them will deliver within 1 week.
Pathophysiology of premature rupture of membrane
The fetal membrane has two layers.
- Inner amnion layer and
- Outer chorion layer
As the pregnancy advance, the fetal membrane will result in structural weakening for different reasons. Some of the reasons are:-
- There will be a change in the intracellular matrix, collagen content, and type.
- Cellular apoptosis
- There is also increased matrix metalloproteinase and decreased tissue inhibitor matrix metalloproteinases.
- The activity of collagenase and protease activity also increases.
The above reasons will result in membrane change which results in membrane rupture.
What are the risk factors?
Different risk factors are associated with PROM. They have been identified to increase the incidence of PROM. Some of them are:-
- Low socioeconomic status
- Any cause which result in uterine overdistention like polyhydramnios and multiple pregnancies,
- Placental Abruption
- Low body mass index
- Nutritional deficiency or copper and ascorbic acid
- Maternal cigarette smoking
- Cervical conization or cerclage
- Pulmonary disease in pregnancy
- Connective tissue disorder
- Preterm labor
- Urogenital tract infection – Neisseria gonorrhea, chlamydia trachomatis, and trichomonas vaginalis. This is due to the direct release of protease and through stimulation or a host inflammatory response increasing local cytokines, metalloprotease, and prostaglandins.
PROM Complications
Maternal complications of premature rupture of membrane
- Chorioamnionitis
- Abruptio placenctae – occur in 4 – 12% of PROM cases.
- Retained placenta
- Post partum hemmorage
- Maternal sepsis – occur in 0.8% of PROM cases.
- Maternal death
- Higher risk of C-section delivery
- Preterm labor
Fetal complications of premature rupture of membrane
- Infection
- Fetal distress
- Cord compression – due to oligohydramnios
- Fetal death
- Premature neonate and complication related to prematurity
- Neonatal sepsis – increase by 2 fold
- Pulmonary hypoplasia – due to oligohydramnios
How do we diagnose premature rupture of membrane?
The main way of diagnosis is clinical evaluation using history and physical examination. On history the mother may complain gush of fluid from the vagina or leakage of liquor may indicate premature rupture of membrane. On physical examination, visualization of amniotic fluid passing through the cervical canal on speculum examination or posterior polling of fluid indicates PROM. The presence of lanugo, vernix cherosa, and meconium is confirmatory.
If we don’t find characteristic features of PROM, we can do other tests like
Nitralizine paper test
Nitralizing paper is a paper which detects the PH difference. It will turn blue if PH is greater than 6 (alkaline environment). And amniotic fluid is alkaline whereas vaginal secretions are acidic. So we will take a sample during speculum examination from posterior fornix then we smear on the neutralizing paper and if it turns blue, that means the fluid is amniotic. In premature rupture of membrane, the pH of the vaginal sidewall or posterior fornix is more than 6 – 6.5.
Some conditions give us a false positive result like blood or semen contamination, alkaline antiseptics, or bacterial vaginosis. These conditions may give us an alkaline environment without the presence of PROM.
Fernin test
Normally if we smear amniotic fluid in the slide and see under a microscope, we will see a leaf-like structure resulted from arborized crystals (ferning) due to the interaction of amniotic fluid proteins and salts. But sometimes cervical mucus can result in the same result.
Indigo carmine test (Confirmatory test)
We can do ultrasound-guided dye infusion into the amniotic fluid through the abdomen (1 ml indigo carmine plus 9 ml sterile saline) then see if there is a stain on the pad. We can’t use methylene blue for this test.
Other supporting tests
Oligohydramnios without urinary tract malformation or fetal growth restriction may suggest membrane rupture.
Management of PROM (Premature rupture of membrane)
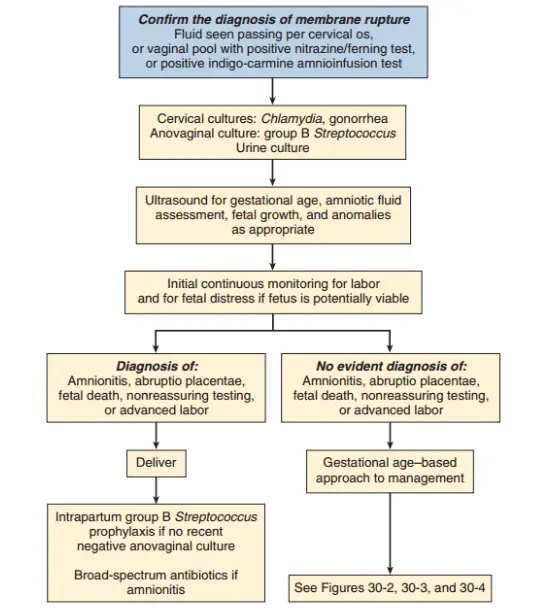
General rules
- The patient should be admitted to a facility capable of emergency delivery if placental abruption or fetal malpresentation or fetal distress occurs. The hospital should have neonatal resuscitation and NICU.
- Avoid digital examination until delivery is inevitable. – it shortens the latency period.
- Narrow-spectrum prophylaxis with intravenous penicillin G – 5 million units intravenous then 2.5 to 3 million units IV every 4 hours. Or ampicillin 2 g IV, then 1 g IV every 4 hours for 48 hours then change it to amoxicillin plus Erythromycin. It significantly prolongs latency period and reduce chorioamnionitis and postpartum endometritis and also prevents newborn complication (neonatal sepsis, pneumonia, and IVH)
- Corticosteroid – either betamethasone 12mg IM every 24 hours (2 doses) or dexamethasone 6mg IM every 12 hours (4 doses). – In preterm PROM, corticosteroid significantly decrease the risk of RDS, IVH, necrotizing enterocolitis without increasing the risk of maternal or neonatal infection.
- PROM management is highly dependent on the gestational age of the pregnancy. It can be classified into:-
- PROM at term (> 37)
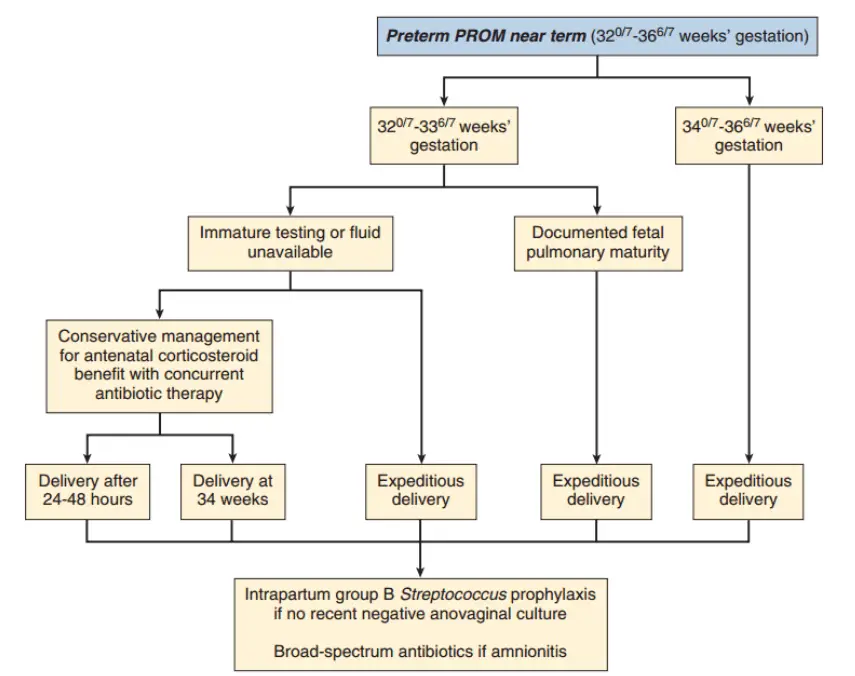
- PROM at near term (GA – 32 – 36)
- Remote from term (GA – 28 – 31 weeks)
Management of PROM at term (> 37)
In this case early delivery is indicated. If labor doesn’t start by itself, induction should be started.
Management of PROM in the near term (GA – 32 – 36)
This further classified into 2.
- If GA – 34 – 36, early delivery is indicted depend on fetomaternal condition.
- If GA – 32 – 33 – antenatal corticosteroid to assist fetal lung maturity if no documented fetal maturity.
Management of PROM remote from term (GA – 28 – 31 weeks)
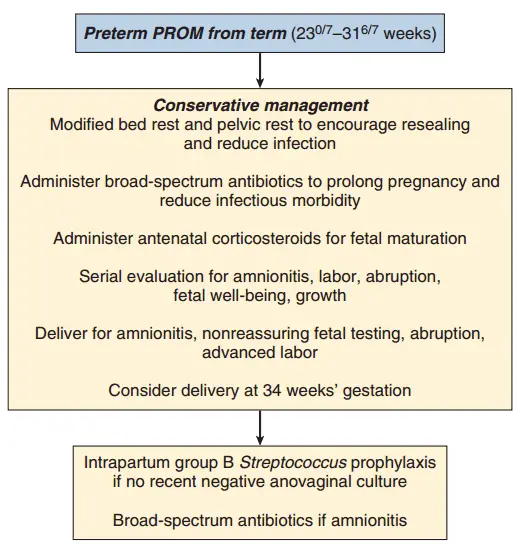
In this case conservative management is a better option. We basicaly wait for the labor to start by itself by doing the following things.
- Follow with prom chart
- Bed rest and pelvic rest – encourage resealing and reduce infection
- Administer broad-spectrum antibiotic – prolong pregnancy and reduce infection
- Administer corticosteroid for fetal maturation
- Deliver at 34 weeks of gestation
- Then give intrapartum GB prophylaxis if no recent negative culture or broad-spectrum antibiotics if there is chorioamnionitis.
When do immediate delivery is indicated?
If there are one of the following conditions, the mother should deliver immediately.
- Chorioaminitis (intra-aminotic infection)
- Intrauterine fetal death
- Cord prolapse
- NRBPP
- Letal congenital anomaly
- Term
- Abruptio placenta
Reference
- Gabbe Obstetrics 6th edition