Placental abruption or abruptio placenta is a detachment of the normally implanted placenta after a period of viability but before the baby is born. The period of viability varies in different countries based on NICU advancement. For instance, the fetus is viable after 20 weeks of gestation in the western world and after 28 weeks of gestation in Developing countries.
The incidence is 1 in 100 births and it attributes about one-third of all antepartum bleeding.
Pathophysiology of placental abruption
Placental abruption is a result of both acute and chronic processes. The initial mild bleeding results in a release of thrombin which plays an important role in the pathogenesis of abruption placenta. More and more bleeding results in adjacent placental ischemia which in turn results in more bleeding.
What are the risk factors of placental abruption?
There are many risk factors associated with placental abruption. Some of them are
Maternal age and parity
As a maternal age advance beyond 35 years of age, the incidence of placental abruption increased. And also as your number of parity (how many times you give birth before) increases, you are at higher risk. In grand multiparous mothers (give birth more than 4 times before), incidence reaches up to 2.5%. This attribute to, the higher the age and the parity of the mother, the higher chance of endometrial injury which will increase the risk of early detachment.
Trauma
Mild to moderate trauma increase the risk by 5%. But in case of severe trauma, the incidence of abruption placenta increase by up to 50%. The most common type of trauma associated with domestic abuse and road traffic accident.
Chronic hypertension and preeclampsia
Maternal hypertension is the most common risk factor that is highly associated with placental abruption. Both increase the risk by 5 fold.
Premature rupture of membrane
PROM increases the risk by up to 5%. It results in intrauterine infection, oligohydramnios, high inflammatory factors like cytokine, a protease which in turn increases the risk of abruption.
On the other way round, thrombin formation during placental abruption will increase the risk of premature rupture of the membrane.
Previous history of abruption placenta
Placental abruption has a recurrence rate of 5 – 17%. After 2 previous histories of placental abruption, the incidence increases by up to 25%.
Smoking and cocaine
Cocaine results in a narrowing of blood vessels and the disruption of vascular integrity. And that in turn increases the risk of placental abruption.
Smoking also highly associates with placental abruption. Compared with non-smokers, smokers have a 40% increased risk of fetal death due to placental abruption. In both cases, the placenta will be hypoperfused so it results in decidual ischemia and necrosis.
Other risk factors
- Uterine malformation or myoma
- Multiple pregnancies
- Increased amniotic fluid (polyhydramnios)
- Thrombophilia
How can we classify placental abruption?
- Depending on the degree of detachment, fetal, and maternal condition, placental abruption is widely classified into three categories.
| Degree of separation | <1/6th | <2/3rd | > or = 2/3rd |
| Amount of vaginal bleeding | < 400 | < 1000 | > or = 1000 |
| Fetal condition | No FHR abnormality | Abnormal FHR | Fetal distress or death |
| Maternal condition | Stable | Postural hypotenstion | Shock |
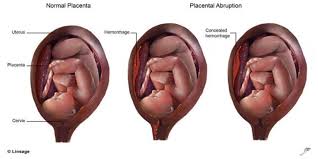
- Depend on detachment type – concealed (20%) or overt
- Based on the temporal nature of abruption – acute versus chronic
- Depend on the location of placental abruption
- Subchorionic – between the planet and the membranes
- Retroplancetal – between the placenta and the myometrium, and
- Preplacental – between the placenta and the amniotic fluid.
What are the signs and symptoms of placental abruption?
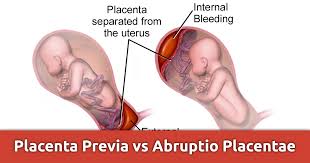
Vaginal bleeding, abdominal pain, and uterine contractions are the three most common symptoms associated with abruptio placenta. The type of bleeding is usually darker, unlike placenta previa. And there will be mild to severe abdominal pain associated with it.
Since 20% of the abrupt placenta is concealed, we can’t estimate a degree of bleeding from the amount of vaginal bleeding.
How do we diagnosis placental abruption?
Abruptio placenta is a diagnosis of exclusion. So we need to exclude other causes that result in bleeding like placenta previa and other local causes.
Clinically
Placental abruption is mostly diagnosed clinically. There are clinical features that are used to differentiate abruption from placenta previa. In abruption placenta, the vaginal bleeding tends to be darker and painful. But in the case of placenta previa, the bleeding is usually bright red and painless.
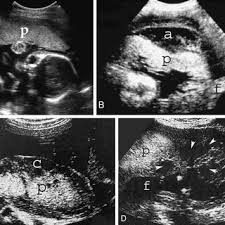
Ultrasound
Ultrasound has little use in diagnosing placental abruption. The main use of ultrasound is
- To exclude placenta previa which is one of the causes of vaginal bleeding (mostly bright red and painless bleeding).
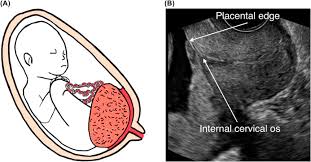
- Ultrasound can predict if the bleeding is acute or chronic. Acute bleeding is more hyper or isoechoic whereas resolving hematoma appears hypoechoic within 1 week.
- It is also used to determine the location of placental abruption.
Others diagnosing tools
- Speculum examination may be needed once placenta previa is excluded with ultrasound. It is useful to exclude local causes.
- Laboratory findings – evidence like hypofibrinogenemia and evidence of consumptive coagulopathy are supportive of severe abruption.
- After C/s is done – there will be a clot visible on the placental surface. You can also predict the degree of detachment this way.
What are the complications of placental abruption?
Maternal Complications
- Hypovolemic shock – due to massive bleeding
- Acute kidney injury – massive bleeding can result in prerenal kidney injury due to decreased blood flow to the kidney.
- DIC – the commonest cause of DIC in pregnancy is abruption placenta.
- Postpartum hemorrhage
- Surgical related complication
Fetal complications
- Prematurity
- Preterm labor
- Non reasuring biophysical profile – fetal distress
- Intrauterine fetal death
- Future neurological sequelle
- Fetal complictions related to c-section delivery
Management options of placental abruption
Depending on the maturity of the fetus, condition of the mother and the fetus, we can manage it accordingly.
Immediate termination
Immediate termination if
- Term fetus or fetal maturity is certain
- Bleeding result in maternal instability (unstable vital signs)
- Labor start
- If the fetus is dead inside the womb (IUFD)
- If there is evident fetal distress
- Severe congenital anomaly of the fetus which is incompatible with life
- Other compications like PROM
Conservative managment
If the above conditions are not present, we continue with conservative management.
- Notify the mother about the condition and consequent management options
- Advice her to rest and avoid coitus
- Follow the patient with APH chart and fetal kick
- Iron therapy for the mother
- Update CBC once or twice weekly
- Prepare OR material by the mother’s side in case an emergency C-section is needed.
- Prepare 2 – 4 units of blood in case the mother needs a transfusion or emergency C-section.
- Steroid (to improve lung maturity of the baby) in case if immediate termination is needed
So if you have any symptoms listed above, you need to get immediate medical attention.
See the video below for more information
Pingback: What Does OBGYN Stand For? When Should I Seek Help? - Life As MD