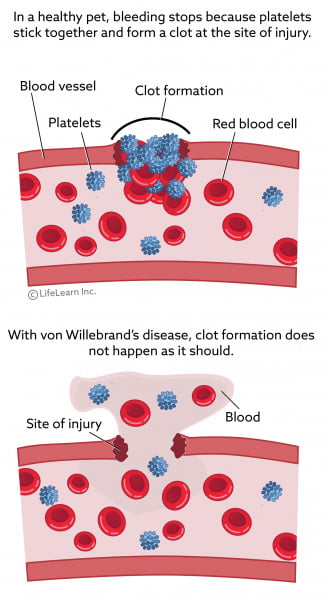
Von Willebrand disease (VWD) is the most common inherited bleeding disorder which is caused by a deficiency of von Willebrand factor in the blood. That means the patinet will have defect in clotting. They tend to bleed more than expected.
What is the von Willebrand factor?
Von Willebrand factor is an important protein in the body that is important for platelet aggregation and blood hemostasis.
VWF act by two mechanisms.
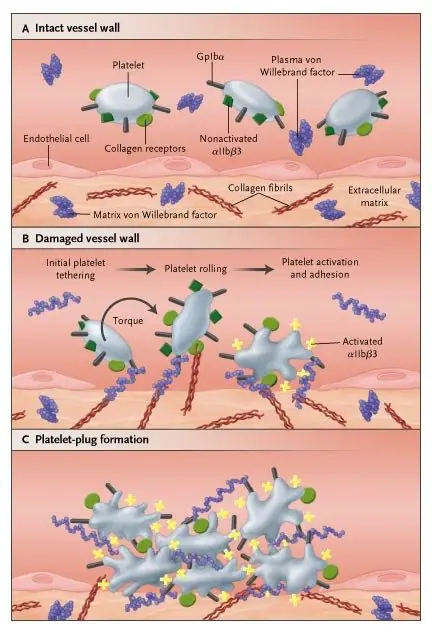
- It serves to tether platelets to injured subendothelium via binding sites for platelets and collagen. So it recruits platelets to the site of clot formation.
- It is a carrier protein for factor VIII. So it protects factor VIII from degradation in plasma.
How common is Von Willebrand disease?
Depending on the criteria used for diagnosis, the prevalence ranged between 1 in 100 to 1 in 10,000.
The incidence between males and female is equal even though women tend to diagnose more than men due to symptoms like menorrhagia.
What are the signs and symptoms of von Willebrand disease?
VWD patients typically presents with mucosal bleeding. They will also have epistaxis, easy bruising, and menorrhagia in women. Due to that women are more likely to be diagnosed.
Some patients may present with anemia symptoms due to chronic and acute bleeding. Anemia symptoms include easy fatiguability, headache, blurring of vision, and tinnitus. In some patients, they might present with petechial and purpural rashes.

Depending on the type of the disease, some patients might present with low platelet, or/and low factor VIII level in the blood. And most of them will have low VWF too.
What factors affect VWD?
VWF is influenced by many factors. For example – blood group O has lower VWF factors. Also, hypothyroidism and medication like valproic acid will result lower VWF factors. On the contrary factors like stress, exercise and pregnancy increase VWF.
Classification of Von willebrand disease?
VWDs are classified depending on quantitative or qualitative defect of VWF. It is classified into 3 types.
- Type 1 VWD – mild to a moderate quantitative defect in VWF
- 2 VWD – a qualitative defect in VWF
- Type 3 VWD – a severe quantitative defect in VWF
Let’s see each of them.
Type 1 VWD
This is the most common type of VWD account for 60 – 80% of the cases. Patients usually present with minor mucosal bleeding, epistaxis, and menorrhagia. And the VWF antigen assay will be below 30 IU/dL.
Type 2 VWD
This type is characterized by decreased VWF activity. Unlike type one and type three VWD, it resulted by the qualitative disfunction of VWF. It can further be classified into five types.
- Type 2A
- Type 2B
- Platelet-type pseudo-VWD
- 2M, and
- 2N
Type 2A
It is caused by a mutation that affects multimer assembly and processing or mutation that result in increased proteolysis of VWF. Symptoms are more severe than type one. And it accounts for 10 percent of VWD cases.
Type 2B
It is caused by the increased ability of VWF to bind platelets. So in this type, both VWf and platelet will decrease.
Platelet-type pseudo-VWD
It is caused by a mutation in platelet glycoprotein Ib which causes spontaneous binding of VWF with platelet. So the patients will have low platelets and VWF.
Type 2M
Here there is decreased VWF activity but near normal multimer distribution.
Type 2N
It caused by a defect in the ability of VWF to bind FVIII.
Type 3 VWD
This is the most severe case of VWD where there is almost no VWF in the system (Factor VIII is less than 10 IU per dL). Due to this, symptoms tend to be more severe like joint bleeding and hemorrhage to the central nervous system.
It is the rare type which occurs only 1 in 1 million population.
How do we diagnose Von Willebrand disease?
What do we find on history and physical examination?
The main complaint of the patient most likely will be bleeding tendency especially minor mucosal bleeding like nasal bleeding and increase menus flow in amount or duration. They most likely have a long history of such complaints.
Some of them can have a family history of minor bleeding or known VWD family member.
On physical examination, the patient may have active mucosal or nasal bleeding. In some severe cases, the patients might even have joint bleeding marked by joint swelling and pain. They may have intracranial bleeding which can be marked by abnormal body movement and loss of consciousness.
Another most common compliant is anemia. Anemic patients usually have pale conjunctiva, tachycardia even ejection systolic murmur at the aortic valve area. The patient might have skin rashes too.
What laboratory investigations are important to diagnose VWD?
- CBC – anemic patinets usually will have low hemoglobin and hematocrit level. And also low platelet level especially in type 2B and platelet type pseudo VWD.
- VWF antigen (VWF: Ag) – measure a total amount of VWF protein.
- Coagulation profile – they might have prolonged partial thromboplastin time since they might have low factor VIII level.
- VWF activity (ristocetin cofactor activity assay / VWF: RCo) – Assess interaction of VWF and platelets as mediated by ristocetin.
- Factor VIII activity – measure circulating FVIII, which will be very low in type 2N and type 3 VWD.
- VWF: RCo / VWF: Ag ratio – decrease ratio (less than 0.7) is found in type 2 VWD.
Treatment of Von Willebrand disease
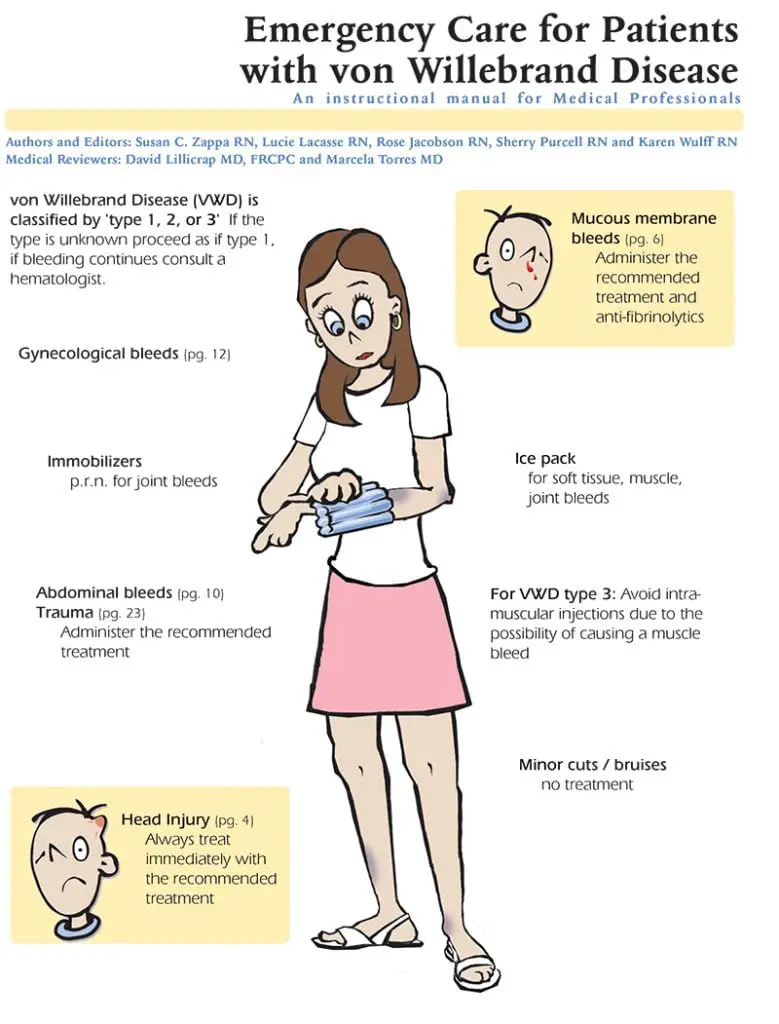
Treatment of VWD highly depends on the type of the disease. For example –
- Desmopressin is a treatment of choice of type one VWD as it increases the amount of circulating VWF by releasing it from storage.
- For type two and three VWD, VWF-containing concentrates is the choice of treatment.
- In some cases platlete transfusion might be needed.
- Adjunct therapy like antifibrinolytic will help for surgery.
- For menorrhagia, we can give hormonal treatment.
- Local treatment for epistasis such as nasal cautery or packing might be helpful.
- In anemic patients, we can provide iron therapy.
Reference
- Nelson textbook of Pediatrics 21st edition