Rh incompatibility means when a mother with RH negative blood type bears an RH positive baby. And Rh sensitization means when the mother produces an antibody against Rh antigen.
Historical background – How Rh antigen Discovered?
During 1940 scientists drow blood from rhesus monkey and inject into a rabbit. The rabbit produced antibodies for a specific (unknown) antigen. Then they took plasma from the rabbit and mix it with human blood then they see an agglutination (reaction).
They called the unknown antigen, RH antigen.

RH antigen is the type of antigen found on blood cells. It comprises 5 types of antigen E,e, C,c, and D. And D antigen is the most potent one. And it can be homozygous (DD) or heterozygous (Dd).
What is Rh Incompatibility?
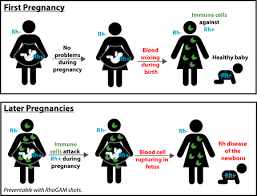
Rh incompatibility means when a mother with RH negative blood type bears an RH positive baby. And Rh Sensitization means when the mother produces an antibody against Rh antigen.
It has different other names like
- RH alloimmunization,
- Rh isoimmunization,
- Hemolytic disease of newborn,
- Erythroblastosis fetalis and so on.
RH sensitization mostly occurs during pregnancy if RH negative woman bearing RH positive fetus. But it also occurs if RH positive blood transfuses to RH negative patient.
Normally fetal RH antigen present by the 38th day after conception. If there is exposure, IgM will be produced by the mother after 6 months. But it can’t cross the placenta because of its big size. That means it doesn’t affect that particular pregnancy. Then after months, IgG will be produced. And it can cross the placenta. So the IgG antibody from the mother will destroy the fetal RBC of the next pregnancy. That is basically what RH isoimmunization is.
But there are some prerequisites should be fulfilled for immunization to occur. These are: –
- Mother should has RH negative blood type and the baby has RH positive blood type,
- Sufficient RBC transferred from the fetus to the mother (> or = 0.1 ml), and
- The mother must be an immunological responder to produce antibody.
Why Some Mothers Don’t Sensitize Even If They Are Exposed?
Some RH negative mothers don’t sensitize even if they are exposed. And there are different reasons for that. Some of the reasons are: –
- if < 0.1 ml blood enters into the mother blood
- 30% of RH negative woman is immunological nonresponders. That means they don’t produce antibodies even if they are exposed.
- insufficient placental transfer of fetal antigen or maternal antibody
- ABO incompatibility is protective against RH sensitization because of two reasons. ABO-incompatible fetal cell cleared from maternal circulation rapidly before they are trapped by the spleen and maternal anti-A or anti-B antibodies damage RH antigen so it is no longer immunogenic. Eg when the mother is type O and the father is type A, B, or AB.
How Does RH Incompatibility Affect Your Pregnancy?
If a mother with RH negative blood type gives birth or abort RH positive baby, she has a 16% risk to be sensitized and that can affect subsequent pregnancies.
Usually, the first pregnancy is spared. Because igG occurs months after exposure. So the effect will be seen in subsequent pregnancies.
It can cause: –
- Hydrops fetalis (accumulation of intravascular fluid in 2 or more fetal compartment) – the most serious complication.
- Jaundice and anemia in neonates (the baby become yellow after birth)
- Congenital anemia of the newborn
- Polyhydramnios (increased aminotic fluid) , IUFD (intrauterine fetal death)
- For the mother, it results in, big baby, increases preeclampsia risk, increased postpartum hemorrhage risk.
What are the Risk Factors?
Risk factors are factors that increase the chance of blood contact between the mother and the fetus in pregnancy.
Such as: –
- Miscarriage
- Amniocentesis
- Abdominal trauma
- Delivery (Mainly Vaginal)
- Cordocentesis
- Abraptio placenta
- Placenta previa with bleeding
- External cephalic version
- Manual removal of placenta
How Can We Diagnose RH Sensitization?
There are 2 tests: –
- Indirect coomb’s test
- Direct coomb’s test
Indirect Coomb’s Test
Blood samples will be taken from the mother and mix with known RH positive blood then mix it with coomb’s serum (anti-human antibody from hourse). Then if the mom is already sensitized (has an antibody against RH antigen), agglutination will occur. That is a positive indirect combat test. If we get a positive test, the next step is to do the titer. The critical titer is 1/32 (some books say 1/16). At this point, the baby has a high risk to develop hydrops fetalis and other complications.
Direct Coomb’s Test
A blood sample will be taken from the baby then it will be mixed with combs reagent. It detects the presence of maternal antibody on neonate RBC. If it agglutinates, we call it a positive test. That means the mother is already sensitized.
How to Prevent RH Sensitization?
3 major steps: –
- Prevent active immunization
- Avoid mismatch transfusion
- Prevent or minimize fetomaternal blood
How To Prevent an Active immunization?
RH anti – D IgG will be administered following birth in 12 days (preferably 72 hours)
The action is it induces antibody-mediated immune suppression. It blocks the RH antigen of fetal cells so it will be removed by the spleen or lymph node without recognized by the mother. it also blocks IgG from B cells by coat fetal RBC.
The does is we give 10 micrograms for every 1 ml of blood transferred. We calculate the transferred blood using Keihauer – Betke test.
Keihauer – Betke test is an acid elution technique to note the number of fetal RBC using a low power field. fetal RBC contains fetal Hgb which is more persistent to acid elution than adult Hgb If there is 20 fetal RBC it represents 1 ml of fetal blood. so we will give 10 micrograms of RH anti – D IgG.
If we can’t estimate the specific amount of blood transferred, we will calculate with 30 ml of blood. so we mostly give 300 microgram dose within 72 hours after giving birth or 50 micrograms in 72 hours after abortion, ectopic or molar pregnancy.
When Do We Give RH anti – D IgG for Prophylaxis?
After we make sure the mother is not sensitized with an indirect combat test, we will give 300 microgram anti – D IgG at the 28th week of gestation. Then repeat the dose within 72 hours after delivery (if the cord blood is Rh-positive).
We will give an additional dose if there are
- Procedures like Amniocentesis, 2nd-trimester chorionic villi sampling,
- If there is hydatid form mole, fetal death in 2nd and 3rd trimester, blunt abdominal trauma, APH, and ECV.
Then we will do an indirect combat test 6 months postpartum to check if prophylaxis was successful. How to avoid mismatch transfusion
We need to check the blood group and Rh factor then do a cross-match before transfusing the patient or the mother.
How to Minimize Fetomaternal Blood?
Some precaution we should follow: –
- We need to avoid routine manual placental removal and minimize spit of blood into the peritoneal cavity during C/s.
- We should also give oxytocin or ergometrine after delivery of the anterior shoulder.
- Do amniocentesis after placenta localized
- Minimize abdominal palpation in abruption-placenta
What If the Mother is Already Sensitized?
- First, do the titer. If the titer is high enough to cause complications,
- Follow with Queenan curve if gestation is before 27 weeks to detect fetal anemia
- Follow with liley graph if gestation if after 28 weeks
- The mother will be followed monthly with amniocentesis (to check bilirubin).
But keep in mind, prevention is better than treatment in this case.
You can ask about RH Incompatibility if you need further explanation and you can also comment on new updates on the topic.

Pingback: What Does OBGYN Stand For? When Should I Seek Help? - Life As MD